Upper Airway Resistance Syndrome
What is UARS (Upper Airway Resistance Syndrome)?

With UARS, there is a restriction of the airflow in the upper airway, but there isn’t a complete blockage. This occurs when the soft tissue in the person’s throat relaxes and impedes the airflow. The airflow is decreased, but not to the degree of OSA. Because it becomes more difficult to breathe, the person will awaken from sleep. He or she may only briefly wake up or they may fully awaken and then have trouble getting back to sleep.
If you want to place UARS, it would fall somewhere between snoring (which is caused when the airway has some resistance from sagging tissue) and OSA. For the person suffering from UARS, their symptoms are similar to OSA in their daytime fatigue, lack of concentration ability, and the like.
What is Obstructive Sleep Apnea?
Obstructive Sleep Apnea, or OSA, is when someone stops breathing for 10 seconds or more while sleeping.
What causes UARS?
UARS occurs when:
- Loose or relaxed fatty tissue in the throat collapses backwards partially blocking the airway
- The tongue falls to the back of the throat, partially blocking airflow
- Improper jaw alignment creates a narrower upper airway
How is UARS different from Sleep Apnea?
The main differentiation is that the UARS patient has more RERAs (Respiratory Effort Related Arousals) during sleep and the OSA patient just stops breathing. UARS is usually recognized by the person her or himself. They will notice they wake at 2 or 3 am and keep watching the clock wondering if they ever slept at all. In OSA, the person will say they sleep very soundly, “like a rock,” and often it is the person’s partner that notices something is wrong-the person stops breathing. Neither of these groups will feel rested or well upon waking. Both of these groups are typically mouth breathers.
How common is Sleep Apnea?
According to data published in the American Journal of Epidemiology, the prevalence of sleep apnea has risen along with the growing obesity rates in the U.S. It’s estimated that one in four adults in the U.S. has obstructive sleep apnea. That equals 67 million people. Yet, of those 67 million, over 53 million (80%) are undiagnosed. They’re going through life feeling tired during the day, suffering from headaches, lacking the ability to focus, or the more serious health conditions described above. Men are at a higher risk for having sleep apnea than women.
What are the symptoms of UARS?
The symptoms of UARS mirror those of obstructive sleep apnea without the more involved possible health considerations such as higher blood pressure and the like. That’s because the abrupt disruption of sleep when the brain wakes the body in OSA is not prevalent with UARS. The symptoms of UARS are similar but less severe.
The typical symptoms of UARS include:
- Snoring
- Daytime sleepiness
- Disturbed or poor sleep
- Trouble returning to sleep once awakened
- Fatigue
- Trouble with concentration
How is UARS diagnosed?
If our doctor, who is a member of the American Academy of Sleep Medicine and the American Academy of Dental Sleep Medicine, suspects a patient may be suffering from UARS, she will have the patient do a polysomnogram, colloquially known as a sleep study. These tests are conducted at a sleep center, where the patient is attached to monitoring equipment. This equipment records these functions:
- Brain waves
- Blood oxygen levels
- Heart rate
- Breathing
- Eye and leg movements
This information can then provide an idea of how much the patient’s sleep is being disturbed or impeded by UARS.
How do you treat UARS?
Treatment options for UARS are similar to those for OSA.
- Oral appliances — This is the first option. There are hundreds of FDA-approved oral appliances that can stop UARS or OSA. These custom appliances are fabricated precisely to fit the patient’s bite. Dental impressions are taken, and these are sent to the oral appliance manufacturer, where the mouth guard is made. When in the patient’s mouth, these appliances place the lower jaw in the correct position to better open the airway in the back of the throat.
- Positive airway pressure — The most popular of these therapies is known as continuous positive airway pressure (CPAP). The patient wears a special mask attached to a machine. The machine gently blows air into the patient’s upper airway, and this difference between the pressure inside the airway and the outer air pressure works to keep the airway open.
- Surgery — Surgery is rarely necessary in cases of UARS, but it can be used to remove some of the tissue in the back of the throat that tends to sag backward and create the air restriction.
Is there recovery after UARS treatment?
 There isn’t any recovery or downtime after treatment for UARS. Patients usually take a night or two to adjust to a new oral appliance, but this doesn’t take long. CPAP machines definitely require some getting used to, as the patient is attached to the machine through their mask and the tubing, but this wouldn’t be deemed “recovery.”
There isn’t any recovery or downtime after treatment for UARS. Patients usually take a night or two to adjust to a new oral appliance, but this doesn’t take long. CPAP machines definitely require some getting used to, as the patient is attached to the machine through their mask and the tubing, but this wouldn’t be deemed “recovery.”
Obviously, there is recovery after oral surgery to reduce throat tissue. These recoveries vary with the procedure used and the extent of the surgery. If this is the necessary treatment path, our doctor will discuss what you could expect after these procedures.
What happens if I don’t treat my Sleep Apnea?
Sleep apnea is misunderstood by many people. Many discount the seriousness of sleep apnea, thinking it’s just a little snoring. That’s a risky line of thinking, going without sleep apnea treatment can lead to a number of very serious health concerns:
- High blood pressure — Because you wake up over and over during the night, this process places stress on your body, activating your hormone systems. This raises your blood pressure.
- Heart disease — People with obstructive sleep apnea are more likely to have heart attacks, strokes, and atrial fibrillation.
- Type 2 diabetes — Sleep apnea is common in people with type 2 diabetes. This is because when your body is tired it has trouble effectively processing insulin.
- Weight gain — Sleep apnea can make your body release more of the hormone ghrelin, which makes you crave carbs and sweets.
- Adult asthma — Adult asthma and sleep apnea combined tend to cause the patient to suffer from more asthma attacks.
- Car accidents — People with sleep apnea are up to five times more likely than normal sleepers to have traffic accidents, and to even fall asleep at the wheel.
What are the risk factors that make it more likely to develop Sleep Apnea?
Certain factors play a role in a person’s being more likely to develop sleep apnea such as being a man, for instance. These are risk factors for obstructive sleep apnea:
- Neck circumference — People with thicker necks often have narrower airways (men 17 inches and larger, women 15 inches and larger).
- Obesity — Obese people have four times the risk of sleep apnea. Fat deposits around the upper airway can add to obstruction.
- Narrowed airway — Some people simply have a naturally narrow throat or have enlarged tonsils or adenoids.
- Men — Men are twice as likely to have sleep apnea.
- Age — Sleep apnea is more common in older adults.
- Family history — Sleep apnea runs in families.
- Smoking — Smokers are three times more likely to have OSA.
- Alcohol or sedatives — These substances relax the throat muscles.
When is it time to contact my doctor about Sleep Apnea?
When you start to notice more serious symptoms of sleep apnea, it’s time to discuss this with your doctor and possibly with our doctor, who is a member of the American Academy of Sleep Medicine and the American Academy of Dental Sleep Medicine. Some of these signs may come from the person sleeping next to you.
- Attention problems
- Irritability
- Excessive daytime sleepiness
- Waking up with a dry mouth or sore throat
- Loud snoring (more prominent with obstructive sleep apnea)
- Abrupt awakenings from sleep
- Episodes of breathing cessation witnessed by another person
- Waking up with a headache in the morning
- Difficulty staying asleep
You’ll be asked to complete a sleep history, usually helped by someone who shares your bed or someone in your household. We likely will also refer you to a sleep disorder center, if it looks like you’re a good candidate. There you will be monitored overnight as you sleep. You may also use a home test, which is a simplified version that measures your heart rate, blood oxygen level, airflow, and breathing patterns while you sleep.
Are there things at home I can do to Improve my Sleep Apnea?
Obstructive sleep apnea can sometimes be improved with certain changes in your lifestyle and behaviors. Our doctor often has her sleep apnea patients work on these areas:
- Lose weight — Even a slight weight loss can relieve constriction in your throat. Getting to your ideal, healthy weight may be all you need to do to open up your airway.
- Exercise — Moderate activity, such as brisk walking, for 30 minutes a day can relieve some symptoms.
- Avoid alcohol, sleeping pills, and tranquilizers — These all relax the muscles in the back of the throat, allowing the sagging that leads to sleep apnea.
- Sleep on your side or abdomen, not your back — Sleeping on your back can cause your tongue and soft palate to rest against the back of your throat, blocking your airway. There are some commercial devices that vibrate when you roll onto your back in sleep.
- Don’t smoke — Smokers are three times more likely to have OSA.
Schedule A Consultation
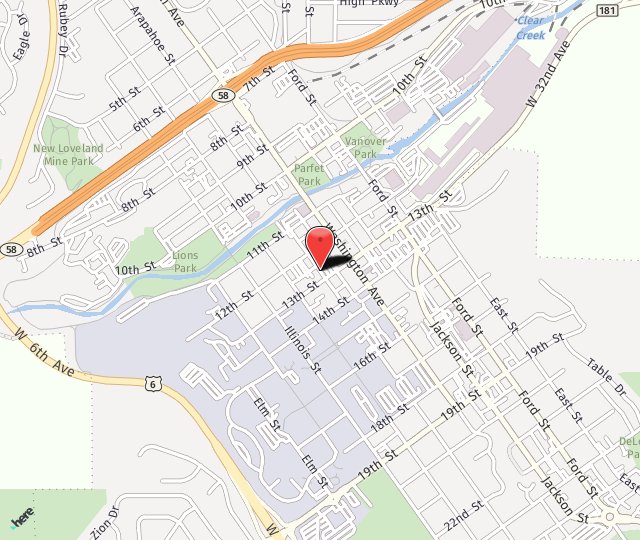
If you are interested in UARS treatment and would like to see if you are a good candidate, call (303) 277-9600 to schedule a consultation. Our practice serves patients from Denver, Arvada, Golden and surrounding areas.

 5 Stars from over 200 reviews!
5 Stars from over 200 reviews!